Easy Stress Free Medical Billing
Call Today 855-561-3214
Medical Billing Services
Do What You Do Best And Leave The Rest To Us
In an ever-evolving healthcare landscape, medical business services play a pivotal role in enhancing operational efficiency for healthcare providers. Our comprehensive suite of services is designed to help medical facilities streamline their processes, enhance patient care, and improve overall financial health. By partnering with us, healthcare organizations can focus more on their core mission—providing exceptional patient care—while we handle the intricate details of their business operations. From billing and coding to regulatory compliance, our expertise ensures that healthcare providers thrive in a competitive environment.
Accuracy in electronic and paper claims within medical billing services is critical for several reasons:
1. Financial Efficiency: Accurate claims ensure that healthcare providers are reimbursed for the services they provided. Inaccuracies can result in underpayment, overpayment, or claim denials, leading to a loss of revenue and increased administrative work to resolve issues.
2. Cash Flow: The promptness of payments is crucial for the financial health of healthcare practices. Accurate claims processing leads to faster reimbursement, helping maintain a steady cash flow.
3. Administrative Burden: Inaccurate claims often result in rejections or require re-submission, which adds to the administrative burden. Staff must spend additional time correcting and resubmitting claims, which could have been used for patient care or other productive activities.
4. Compliance: Healthcare providers must comply with various laws and regulations regarding billing practices. Accurate claim submission helps ensure compliance with these regulations and avoids potential legal issues or penalties.
5. Patient Satisfaction: Inaccuracies in billing can also affect patients, who may be billed incorrectly or face delays in claim processing. Accurate claims contribute to a positive experience for patients, who are less likely to encounter billing issues.
Proper payment posting is a crucial element in the medical billing process:
1. Accuracy of Financial Records: Strong payment posting procedures ensure that financial records reflect actual transactions accurately. This includes the correct application of payments, adjustments, and write-offs to patient accounts.
2. Revenue Cycle Management: Payment posting is an integral part of the revenue cycle management (RCM), which tracks revenue from patients from their initial appointment or registration through to the final payment of balance. Accurate payment posting contributes to effective RCM by providing clear and precise data on actual revenue.
3. Contractual Compliance: The payment posting process involves applying adjustments and write-offs according to the contractual agreements with payers. This ensures that the amounts billed, adjusted, and written off are in line with agreed-upon terms with insurance companies.
4. Error Identification: The payment posting process can help in identifying trends in denials or underpayments, which can then be addressed to improve the efficiency of the medical billing process.
5. Auditing and Compliance: Payment posting records are important for auditing purposes and compliance with regulatory requirements. Accurate payment posting helps ensure that a practice is prepared for any audits by insurance companies or regulatory bodies.

Medical billing insurance follow-ups and why it is critical:
1. Financial Stability of the Hospital: Effective A/R follow-up ensures that claims are paid and receives the funds it is due. This is vital for maintaining financial stability and covering operational costs.
2. Recovering Overdue Payments: A/R follow-ups are key to identifying and recovering overdue payments. By actively pursuing these payments, healthcare providers can reduce the amount of outstanding A/R and improve their financial situation.
3. Maintaining Cash Flow: Timely follow-up on unpaid claims helps maintain a steady cash flow for the healthcare provider. This is essential for the provider to meet its financial obligations, like payroll, supplies, and other operational expenses.
4. Reducing the Age of A/R: A/R follow-up efforts help in reducing the age of accounts receivable by ensuring that claims are processed and paid promptly. A lower average age of A/R is typically indicative of a more efficient billing process and healthier revenue cycle.
Heading
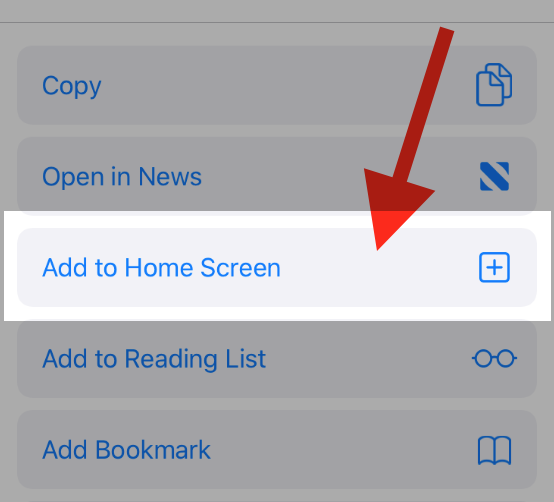
To add this web app to your homescreen, click on the "Share" icon
![]()
Then click on "Add to Home"
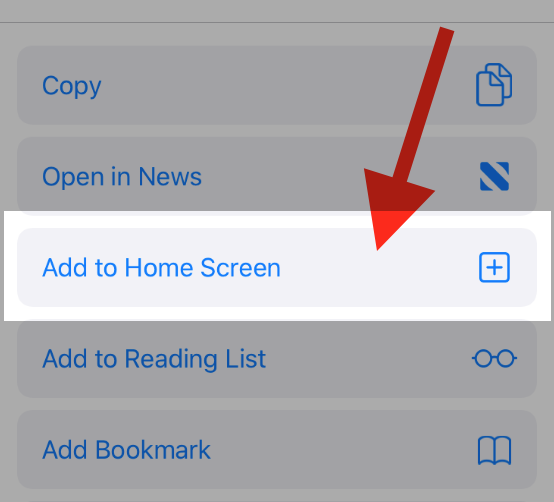
To add this web app to your homescreen, click on the "Share" icon
![]()
Then click on "Add to Home"
It looks like your browser doesn't natively support "Add To Homescreen", or you have disabled it (or maybe you have already added this web app to your applications?)
In any case, please check your browser options and information, thanks!
It looks like your browser doesn't natively support "Add To Homescreen", or you have disabled it (or maybe you have already added this web app to your applications?)
In any case, please check your browser options and information, thanks!